Navigating GRAS Panels: A Guide to Best Practices

When it comes to introducing new substances into the world of food and dietary supplements, ensuring safety is paramount. The GRAS (Generally Recognized as Safe) designation plays a critical role in this process. The U.S. Food and Drug Administration (FDA) provides guidance on how to convene a GRAS panel effectively and responsibly, ensuring that the
... Read moreUnderstanding FDA FURLS, FDA Approved, and FDA Registered Medical Devices
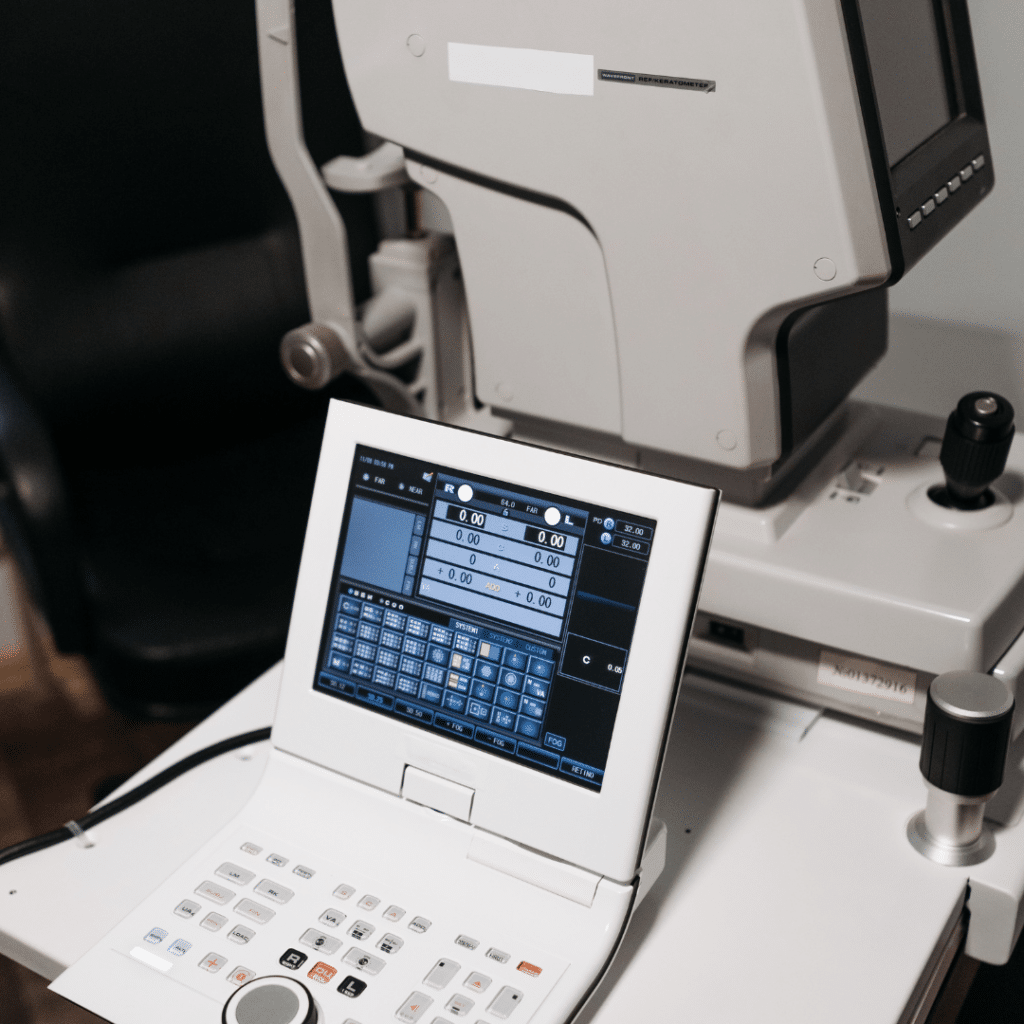
This article explores the differences between these designations and provides insights into how to obtain the necessary licenses for medical devices.
... Read moreCritical Control Points Explained: The Core of HACCP

Learn about Critical Control Points (CCPs) in HACCP, their role in food safety, and how to stay compliant with global regulations.
... Read more